Limit of Premature Viability — A Comparison of Several Countries: A Systematic Review
Main Article Content
Abstract
Background
The objective was to carry out a systematic analysis of mortality in preterm infants from different countries to answer the question about which countries have the highest and lowest survival rates for extremely premature newborns.
Methods
The systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines with which articles, drawn from sources such as PubMed, ScienceDirect and Google Scholar and published between 2016 and 2021, were analyzed. Pregnancies up to 37 weeks of gestation were considered.
Results
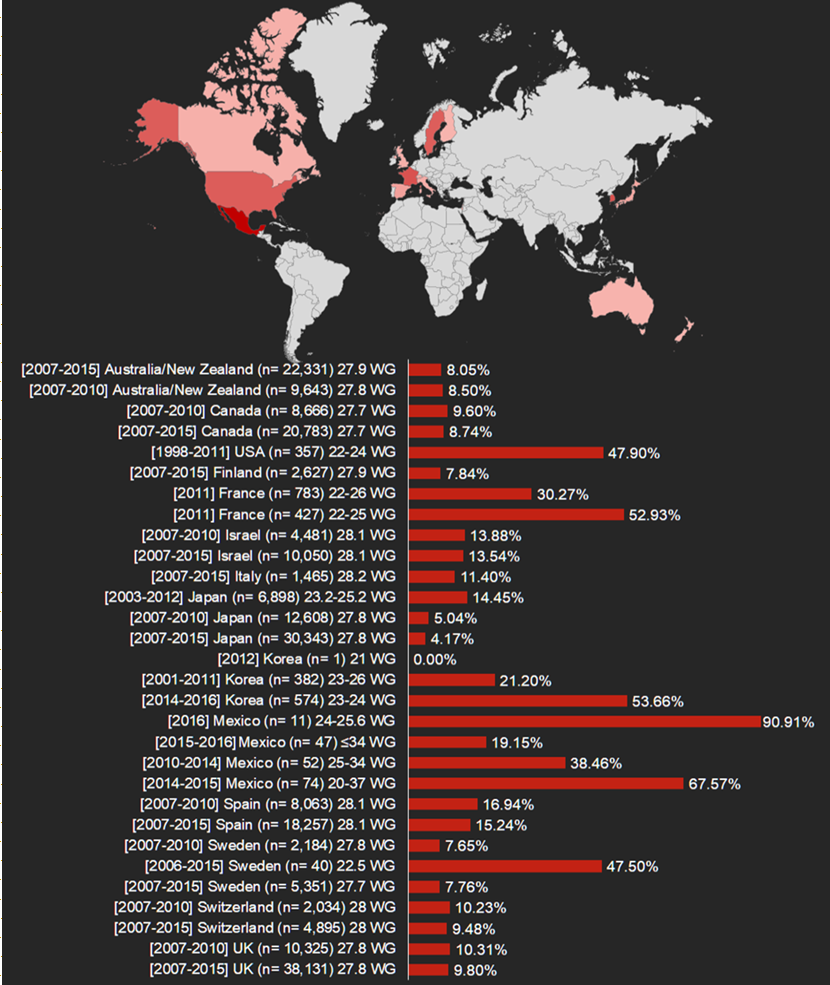
Out of a total of 7,908 articles with the research terms, 14 articles were included. The most extreme prematurity case occurred in Korea with a female newborn of 21 weeks of gestation. The results show that high income countries fared better than low-income countries in securing low mortality rates. These countries include Japan (4.17%), Sweden (7.65%) and Finland (7.84%). In contrast, low-income countries were less able to manage the incidence of mortality among premature babies. Another notable finding was an extreme case of prematurity which occurred in Korea with a female of 21 weeks of gestation.
Conclusion
Mexico has one of the highest mortality percentages among extreme premature newborns. Possibly, the economic development of each country determines the number of resources allocated to the care of premature neonates which determines survival rates. On the other hand, each country has different therapeutic approaches, legal and ethical frameworks, and may offer proactive therapy or counseling to parents to provide palliative care.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) license. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
How to Cite
References
American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care consensus No. 6: Periviable Birth. Obstet Gynecol. 2017;130(4):e187-e199. Doi: 10.1097/AOG.0000000000002352 PMID: 28937572
WHO. 2018. Preterm birth. https://www.who.int/news-room/fact-sheets/detail/preterm-birth.
Perinatal Palliative Care: ACOG COMMITTEE OPINION, Number 786. Obstet Gynecol. 2019;134(3):e84-e89. Doi: 10.1097/AOG.0000000000003425 PMID: 31441826
WHO. 2015. Recommendations on Interventions to Improve Preterm Birth Outcomes. Geneva: World Health Organization; (WHO Guidelines Approved by the Guidelines Review Committee). http://www.ncbi.nlm.nih.gov/books/NBK321160.
Committee on Obstetric Practice. Committee Opinion No. 713: Antenatal Corticosteroid Therapy for Fetal Maturation. Obstet Gynecol. 2017;130(2):e102-e109. Doi: 10.1097/AOG.0000000000002237 PMID: 28742678
Meller CH, Carducci ME, Ceriani Cernadas JM, Otaño L. Preterm premature rupture of membranes. Arch Argent Pediatr. 2018;116(4):e575-e581. Doi: 10.5546/aap.2018.eng.e575 PMID: 30016035
Alison M, Tilea B, Toumazi A, Biran V, Mohamed D, Alberti C, et al; PREMILOC Trial group. Prophylactic hydrocortisone in extremely preterm infants and brain MRI abnormality. Arch Dis Child Fetal Neonatal Ed. 2020;105(5):520-525. Doi: 10.1136/archdischild-2019-317720 PMID: 31980445
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Doi: 10.1136/bmj.n71 PMID: 33782057
Moola S, Munn Z, Sears K, Sfetcu R, Currie M, Lisy K, Tufanaru C, Qureshi R, Mattis P, Mu P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute's approach. Int J Evid Based Healthc. 2015;13(3):163-9. Doi: 10.1097/XEB.0000000000000064. PMID: 26262566.
Lui K, Lee SK, Kusuda S, Adams M, Vento M, Reichman B, et al; International Network for Evaluation of Outcomes (iNeo) of neonates Investigators. Trends in Outcomes for Neonates Born Very Preterm and Very Low Birth Weight in 11 High-Income Countries. J Pediatr. 2019;215:32-40.e14. Doi: 10.1016/j.jpeds.2019.08.020 Erratum in: J Pediatr. 2021 Jun;233:294-299. PMID: 31587861
Shah PS, Lui K, Sjörs G, Mirea L, Reichman B, Adams M, et al; International Network for Evaluating Outcomes (iNeo) of Neonates. Neonatal Outcomes of Very Low Birth Weight and Very Preterm Neonates: An International Comparison. J Pediatr. 2016;177:144-152.e6. Doi: 10.1016/j.jpeds.2016.04.083 PMID: 27233521
Younge N, Smith PB, Gustafson KE, Malcolm W, Ashley P, Cotten CM, et al. Improved survival and neurodevelopmental outcomes among extremely premature infants born near the limit of viability. Early Hum Dev. 2016;95:5-8. Doi: 10.1016/j.earlhumdev.2016.01.015 PMID: 26900775
Diguisto C, Foix L'Helias L, Morgan AS, Ancel PY, Kayem G, Kaminski M, et al. Neonatal Outcomes in Extremely Preterm 10.1038/s41390-021-01375-z PMID: 33504968.
Sung SI, Ahn SY, Yoo HS, Chang YS, Park WS. The Youngest Survivor with Gestational Age of 21⁵/₇ Weeks. J Korean Med Sci. 2018;33(3):e22. Doi: 10.3346/jkms.2018.33.e22 PMID: 29215809
Park JH, Chang YS, Sung S, Ahn SY, Park WS. Trends in Overall Mortality, and Timing and Cause of Death among Extremely Preterm Infants near the Limit of Viability. PLoS One. 2017;12(1):e0170220. Doi: 10.1371/journal.pone.0170220 PMID: 28114330.
Park JH, Chang YS, Sung S, Park WS; Korean Neonatal Network. Mortality Rate-Dependent Variations in the Timing and Causes of Death in Extremely Preterm Infants Born at 23-24 Weeks' Gestation. Pediatr Crit Care Med. 2019;20(7):630-637. Doi: 10.1097/PCC.0000000000001913 PMID: 31013260
Carrera-Muiños S, Cardona-Pérez JA, Fernández-Carrocera LA, Corral-Kassian E, Coronado-Zarco IA, Yllescas Medrano E. Determinación de los límites de viabilidad al nacimiento. Revista Latinoamericana de Perinatología. 2016;19:72–76.
Martínez SM, Vázquez ENC, Delfín IN, Cabrera CV, Azuara MGM, Vázquez GSA. Factores de mortalidad en prematuros menores de 34 semanas de gestación. Acta Pediátrica México. 2021;42(2):66–73.
Montaño-Pérez CM, Cázarez-Ortiz M, Juárez-Astorga A, Ramírez-Moreno MA. Morbilidad y mortalidad en recién nacidos menores de 1,000 gramos en una institución pública de tercer nivel en México. Revista mexicana de pediatría. 2019;86(3):108-111.
Esparza-Valencia DM, Toro-Ortiz JC, Hernández-Rodríguez HG, Herrera-Ortega O, de la Maza-Labastida S, Fernández-Lara JA. Tasa de nacimientos y sobrevida de neonatos pretérmino con peso ≤ 1000 g en un hospital de segundo nivel de San Luis Potosí, México. Ginecología y Obstetricia de México. 2017;84(10), 645–651.
Backes CH, Söderström F, Ågren J, Sindelar R, Bartlett CW, Rivera BK, et al. Outcomes following a comprehensive versus a selective approach for infants born at 22 weeks of gestation. J Perinatol. 2019;39(1):39-47. Doi: 10.1038/s41372-018-0248-y PMID: 30353079
Vu HD, Dickinson C, Kandasamy Y. Sex Difference in Mortality for Premature and Low Birth Weight Neonates: A Systematic Review. Am J Perinatol. 2018;35(8):707-715. Doi: 10.1055/s-0037-1608876 PMID: 29241280
Tottman AC, Oliver CJ, Alsweiler JM, Cormack BE. Do preterm girls need different nutrition to preterm boys? Sex-specific nutrition for the preterm infant. Pediatr Res. 2021;89(2):313-317. Doi: 10.1038/s41390-020-01252-1 PMID: 33184497
Connolly M, Phung L, Farrington E, Scoullar MJL, Wilson AN, Comrie-Thomson L, et al. Defining Preterm Birth and Stillbirth in the Western Pacific: A Systematic Review. Asia Pac J Public Health. 2021;33(5):489-501. Doi: 10.1177/10105395211026099 PMID: 34165364.
Patel RM. Short- and Long-Term Outcomes for Extremely Preterm Infants. Am J Perinatol. 2016;33(3):318-28. Doi: 10.1055/s-0035-1571202 PMID: 26799967
Rivera-Rueda MA, Fernández-Carrocera LA, Michel-Macías C, Carrera-Muiños S, Arroyo-Cabrales LM, Coronado-Zarco IA, et al. Morbilidad y mortalidad de neonatos < 1,500 g ingresados a la UCIN de un hospital de tercer nivel de atención. Perinatología y Reproducción Humana, 2017;31(4):163–169.
Carvalho WB, Matsushita FY, Krebs VLJ. Gray zone: mortality profile of newborns at the limit of viability. Rev Assoc Med Bras (1992). 2019;65(9):1128-1129. Doi: 10.1590/1806-9282.65.9.1128 PMID: 31618324
De Proost L, Ismaili M'hamdi H, Verhagen AAEE, Reiss I, Geurtzen R, Verweij EJJ. On the limits of viability: toward an individualized prognosis-based approach. J Perinatol. 2020;40(12):1736-1738. Doi: 10.1038/s41372-020-00793-x PMID: 32826936
Chen YJ, Yu WH, Chen LW, Huang CC, Kang L, Lin HS, et al. Improved Survival of Periviable Infants after Alteration of the Threshold of Viability by the Neonatal Resuscitation Program 2015. Children (Basel). 2021;8(1):23. Doi: 10.3390/children8010023 PMID: 33406755
Lincetto O, Banerjee A. World Prematurity Day: improving survival and quality of life for millions of babies born preterm around the world. Am J Physiol Lung Cell Mol Physiol. 2020;319(5):L871-L874. Doi: 10.1152/ajplung.00479.2020. PMID: 33050711.