Factors Associated with the Utilization of Healthcare Services in Osun State: Implication for Enrolment into Health Insurance Scheme
Main Article Content
Abstract
Background
Millions of Nigerians are unable to access healthcare due to the high cost and lack of health insurance, resulting in significant out-of-pocket expenses. The government introduced health insurance to reduce financial hardship and move toward universal health coverage. This study aimed to determine the factors associated with the utilization of healthcare services in Osun State with implications for enrolling in the health insurance scheme.
Methods
This was an analytical cross-sectional study of 420 respondents selected using the multistage sampling method. A structured interviewer-administered questionnaire was used to elicit data. Composite variables for healthcare service utilization were computed from the questionnaire and categorized as good or poor for both enrolled and non-enrolled respondents. Data analysis was done using IBM SPSS version 24, and p ≤ 0.05 was taken as statistically significant.
Results
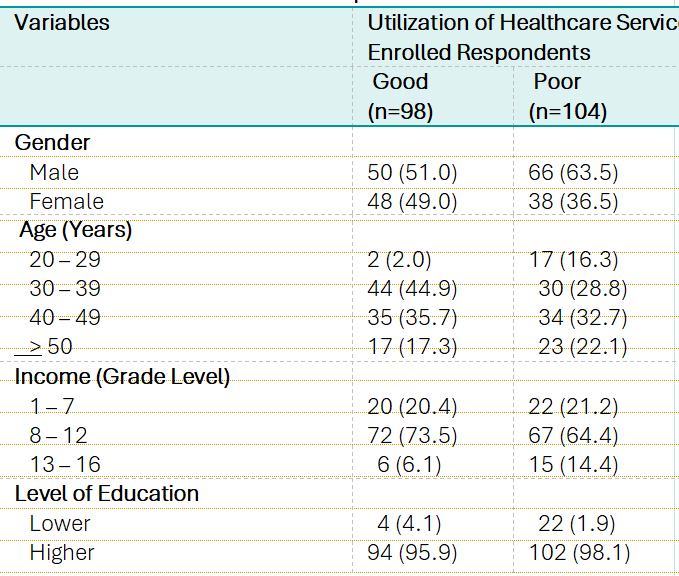
A significantly higher proportion of enrolled respondents utilized healthcare services compared to the non-enrolled (90.2%, p < 0.001). Good utilization among enrollees was associated with age 40–49 (34.1%, p = 0.001), higher income (p = 0.004), larger households (p = 0.028), and more dependents (p = 0.054). Among non-enrollees, age 30–39 (44.9%, p = 0.002) and larger households (74.5%, p = 0.052) also showed higher utilization. Income level significantly predicted utilization for both enrollees (OR = 6.875, CI = 1.056–44.778) and non-enrollees (OR = 2.579, CI = 1.111–5.987).
Conclusion
Health insurance enrollment improves access to healthcare and reduces financial burden. Lack of enrollment may worsen barriers to care. The government should expand coverage to include a larger portion of the workforce and the general population in order to achieve universal health coverage.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) license. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
How to Cite
References
Liaropoulos L, Goranitis I. Health care financing and the sustainability of health systems. International Journal for Equity in Health. 2015;14:5–8.
Syafinaz I, Juni MH, Wan A, Sze D. Health care provision and equity. International Journal of Public Health and Clinical Sciences. 2016;3.
Healthy Systems for Universal Health Coverage: A Joint Vision for Healthy Lives. Healthy Systems for Universal Health Coverage: A Joint Vision for Healthy Lives. 2018;
Wonde D, Tadele G. Impediments of health seeking behavior and health service utilization from healthcare facilities in a rural community in East Gojjam Zone , Ethiopia. The Ethiopian Journal of Health Development. 2015;29.
Mitričević S, Janković J, Stamenković Ž, Bjegović-Mikanović V, Savić M, Stanisavljević D, et al. Factors influencing utilization of preventive health services in primary health care in the Serbia. International Journal of Environmental Research and Public Health. 2021;18(6):1–12.
Vt I, Oom O, Jc N, Vy A, Adam VY. Perceptions and Factors affecting Utilization of Primary Health Care Services in a predominantly Urban Community in South-South Nigeria. 2023;22(2):38–46.
National Academies of Sciences, Engineering, and Medicine Committee on Health Care Utilization and Adults with Disabilities. Health-Care Utilization as a Proxy in Disability Determination. 2018.
Levesque JF, Harris MF, Russell G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. International Journal for Equity in Health. 2013;12(1):1–9.
Onah MN, Govender V. Out-of-Pocket Payments , Health Care Access and Utilisation in South-Eastern Nigeria : A Gender Perspective. 2014;9(4).
Enemuwe IM, Oyibo P. Prevalence and predictors of catastrophic health expenditure due to out ‑ of ‑ pocket payment among rural households in Delta State , Nigeria : a community ‑ based cross ‑ sectional study. Discover Health Systems. 2025;
Edeh HC. Exploring dynamics in catastrophic health care expenditure in Nigeria. Health Economics Review. 2022;12(1):1–20.
Etiaba E, Okwuosa C, Envuladu E, Onwujekwe OE. Health care financing in Nigeria : Implications for achieving universal health coverage. 2015;18(4):437–44.
Sriram S, Khan MM. Effect of health insurance program for the poor on out-of-pocket inpatient care cost in India: Evidence from a nationally representative cross-sectional survey. BMC Health Services Research. 2020;20(1):1–21.
Onwujekwe O, Ezumah N, Mbachu C, Obi F, Ichoku H, Uzochukwu B, et al. Exploring effectiveness of different health financing mechanisms in Nigeria ; what needs to change and how can it happen ? 2019;4:1–13.
Amedari MI, Ejidike IC. Improving access, quality and efficiency in health care delivery in Nigeria: a perspective. Pan African Medical Journal One Health. 2021;5(May).
Iyalomhe FO, Adekola PO, Cirella GT. Community-based health financing: empirical evaluation of the socio-demographic factors determining its uptake in Awka, Anambra state, Nigeria. International Journal for Equity in Health. 2021;20(1):1–13.
Dassah E, Aldersey H, Mccoll MA, Davison C. Factors affecting access to primary health care services for persons with disabilities in rural areas : a “ best-fit ” framework synthesis. 2018;1–13.
Adebiyi O, Adeniji FO. Factors Affecting Utilization of the National Health Insurance Scheme by Federal Civil Servants in Rivers State , Nigeria. 2021;
Akinyemi OO, Owopetu OF, Agbejule IO. National Health Insurance Scheme : Perception and Participation of Federal Civil Servants in Ibadan. Annals of Ibadan postgraduate medicine. 2021;19(1):49–55.
Osei Afriyie D, Krasniq B, Hooley B, Tediosi F, Fink G. Equity in health insurance schemes enrollment in low and middle-income countries: A systematic review and meta-analysis. International Journal for Equity in Health. 2022;21(1):1–12.
Hooley B, Afriyie DO, Fink G, Tediosi F. Health insurance coverage in low-income and middle-income countries: progress made to date and related changes in private and public health expenditure. BMJ Global Health. 2022;7(5):e008722.
Abubakar I, Dalglish SL, Angell B, Sanuade O, Abimbola S, Adamu AL, et al. The Lancet Nigeria Commission: investing in health and the future of the nation. The Lancet. 2022;399(10330):1155–200.
Esan OT, Falayi KO, Adekunle BA, Akinwunmi T, Ajao OO, Abubakar Y. Willingness of in ‑ patients to Uptake the Vital Contributor Social Health Insurance Program in a Teaching Hospital , Southwest Nigeria. Nigerian Journal of Medicine. 2020;1–13.
James N, Acharya Y. Increasing Health Insurance Enrollment in Low- and Middle-Income Countries: What Works, What Does Not, and Research Gaps: A Scoping Review. Inquiry (United States). 2022;59.
Mosadeghrad AM. Factors influencing healthcare service quality. International Journal of Health Policy and Management. 2014;3(2):77–89.
Ewelukwa O, Onoka C, Onwujekwe O. Viewing health expenditures, payment and coping mechanisms with an equity lens in Nigeria. BMC health services research. 2013;13:87.
Leck I. Methods in observational epidemiology. Vol. 41, Journal of Epidemiology & Community Health. 1987. p. 263–4.
Olugbenga-Bello AI, Adebimpe WO. Knowledge and attitude of civil servants in osun state, southwestern nigeria towards the national health insurance. Nigerian Journal of Clinical Practice. 2010;13(4):421–6.
Sanusi R.A AA. An Assessment of Awareness Level of NHIS Among Health Care Consumers in Oyo State, Nigeria.pdf. MEDWELL PUBLISHING; 2009.
Abel AO. Level and Correlates of Health Insurance Coverage in Nigeria : Evidence from 2013 Nigeria Demographic and Health Survey . 2018;7:16–27.
Lokotola CL, Mash R, Sethlare V, Shabani J, Temitope I, Baldwin-ragaven L, et al. Migration and primary healthcare in sub-Saharan Africa : A scoping review. African Journal of Primary Health Care & Family Medicine. 2024;1–10.
Badu E, Agyei-baffour P, Acheampong IO, Opoku MP, Addai-donkor K. Households Sociodemographic Profile as Predictors of Health Insurance Uptake and Service Utilization : A Cross-Sectional Study in a Municipality of Ghana. 2018;2018.
Amu H, Dickson KS, Kumi-Kyereme A, Maafo Darteh EK. Understanding variations in health insurance coverage in Ghana, Kenya, Nigeria, and Tanzania: Evidence from demographic and health surveys. PLoS ONE. 2018;13(8):1–14.
Erinoso O, Oyapero A, Familoye O, Omosun A, Adeniran A, Kuyinu Y. Predictors of health insurance uptake among residents of Lagos, Nigeria. Population Medicine. 2023;5(July):1–7.
Ibok N. Socio-Economic and Demographic Determinants of Health Insurance Consumption. Canadian Social Sciences. 2012;8(5):58–64.
Nkatha L. Macroeconomic Determinants of Health Insurance Demand in Kenya : An Autoregressive Distributed Lag Modelling. The International Journal of Humanities and Social Studies. 2022;8(2):65–74.
Kuwawenaruwa A, Ramsey K, Binyaruka P, Baraka J, Manzi F, Borghi J. Implementation and effectiveness of free health insurance for the poor pregnant women in Tanzania_ A mixed methods evaluation - PubMed. Social Science and Medicine. 2019;225:17–25.
Sanogo NA, Fantaye AW, Yaya S. Beyond coverage : a qualitative study exploring the perceived impact of Gabon ’ s health insurance plan on access to and quality of prenatal care. 2020;6:1–16.
Aziz N, Liu T, Yang S. Causal relationship between health insurance and overall health status of children : Insights from Pakistan. Frontiers in Public Health. 2022;10.
Azzani M, Roslani AC, Su TT. Determinants of household catastrophic health expenditure: A systematic review. Malaysian Journal of Medical Sciences. 2019;26(1):15–43.