Effectiveness of Chlorhexidine – Alcohol Compared with Povidone Iodine for Preventing Surgical Site Infection: A Randomized Trial
Main Article Content
Abstract
Background
Common agents for surgical site skin preparation are povidone iodine and alcohol based chlorhexidine /Cetrimide. The effectiveness of one over the other remains debatable. Our objective was to determine the effectiveness of alcohol-based chlorhexidine/cetrimide mixture compared with povidone iodine for preventing surgical site infection
Methods
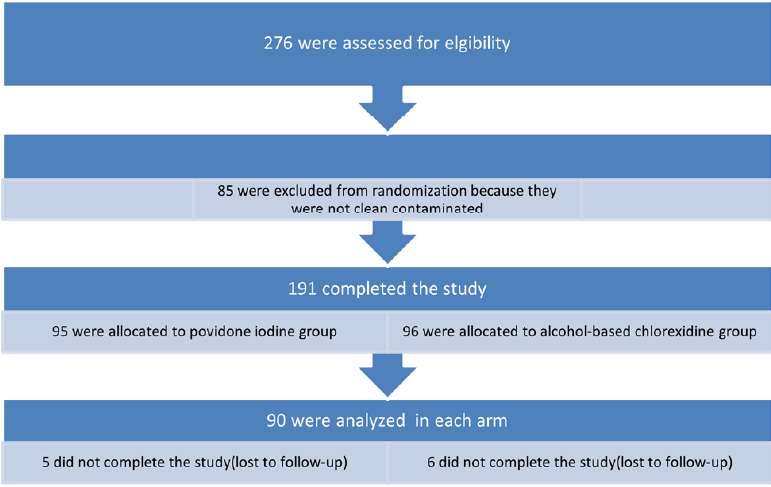
All clean contaminated general and urological surgeries were recruited into the study. Patients were randomized into two groups (A & B) using GraphPad Cals. Alcohol-based chlorhexidine/cetrimide solution was assigned group A while povidone iodine solution was assigned group B. The rate of surgical site infection in each group was compared using hi-squared test. P < 0.05 was considered statistically significant.
Results
A total of 90 patients were allocated to each group of povidone iodine and alcohol based – chlorhexidine/cetrimide mixture/.The duration of the procedures ranged from 0.5-3hours in the povidone iodine group with a mean of 1.28 +/0.81 hours, and from 0.5 to 4 hours in the alcohol –chlorhexidine/ cetrimide mixture group, with a mean of 1.9 +/ 1.03 hours. The rate of surgical site infection among the povidone iodine and alcohol – chlorhexidine/cetrimide mixture group were 5.5% and 1.6% (relative risk RR=0.3) respectively. (p< 0.001).
Conclusions
This study has established that the rate of SSI was lower in patients that had alcohol–chlorhexidine/cetrimide skin preparation. This may be a pointer to the effectiveness of alcohol-based chlorhexidine/cetrimide mixture compared to povidone iodine. Lower incidence of SSI may lead to reduction in post-operative hospital stay.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) license. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
How to Cite
References
Owens C, Stoessel K. Surgical site infections: epidemiology, microbiology and prevention. Journal of hospital infection. 2008;70:3-10. DOI: https://doi.org/10.1016/S0195-6701(08)60017-1
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infection Control & Hospital Epidemiology. 1992;13(10):606-8. DOI: https://doi.org/10.2307/30148464
Mawalla B, Mshana SE, Chalya PL, Imirzalioglu C, Mahalu W. Predictors of surgical site infections among patients undergoing major surgery at Bugando Medical Centre in Northwestern Tanzania. BMC surgery. 2011;11(1):1-7. DOI: https://doi.org/10.1186/1471-2482-11-21
Jenks P, Laurent M, McQuarry S, Watkins R. Clinical and economic burden of surgical site infection (SSI) and predicted financial consequences of elimination of SSI from an English hospital. Journal of Hospital infection. 2014;86(1):24-33. DOI: https://doi.org/10.1016/j.jhin.2013.09.012
Akhter MSJ, Verma R, Madhukar KP, Vaishampayan AR, Unadkat P. Incidence of surgical site infection in postoperative patients at a tertiary care centre in India. Journal of wound care. 2016;25(4):210-7. DOI: https://doi.org/10.12968/jowc.2016.25.4.210
Henriksen N, Meyhoff C, Wetterslev J, Wille-Jørgensen P, Rasmussen L, Jorgensen L, et al. Clinical relevance of surgical site infection as defined by the criteria of the Centers for Disease Control and Prevention. Journal of Hospital Infection. 2010;75(3):173-7. DOI: https://doi.org/10.1016/j.jhin.2009.12.022
Kolasiński W. Surgical site infections–review of current knowledge, methods of prevention. Polish Journal of Surgery. 2019;91:41-7.
Maiwald M, Widmer AF. WHO's recommendation for surgical skin antisepsis is premature. The Lancet Infectious Diseases. 2017;17(10):1023-4. DOI: https://doi.org/10.1016/S1473-3099(17)30448-6
Allegranzi B, Egger M, Pittet D, Bischoff P, Nthumba P, Solomkin J. WHO's recommendation for surgical skin antisepsis is premature–Authors' reply. The Lancet Infectious Diseases. 2017;17(10):1024-5. DOI: https://doi.org/10.1016/S1473-3099(17)30526-1
Monahan M, Jowett S, Pinkney T, Brocklehurst P, Morton DG, Abdali Z, et al. Surgical site infection and costs in low-and middle-income countries: A systematic review of the economic burden. PloS one. 2020;15(6):e0232960. DOI: https://doi.org/10.1371/journal.pone.0232960
Royle R, Gillespie BM, Chaboyer W, Byrnes J, Nghiem S. The burden of surgical site infections in Australia: A cost-of-illness study. Journal of Infection and Public Health. 2023;16(5):792-8. DOI: https://doi.org/10.1016/j.jiph.2023.03.018
Kaye KS, Schmit K, Pieper C, Sloane R, Caughlan KF, Sexton DJ, et al. The effect of increasing age on the risk of surgical site infection. The Journal of infectious diseases. 2005;191(7):1056-62. DOI: https://doi.org/10.1086/428626
Bischoff P, Kramer TS, Schröder C, Behnke M, Schwab F, Geffers C, et al. Age as a risk factor for surgical site infections: German surveillance data on total hip replacement and total knee replacement procedures 2009 to 2018. Eurosurveillance. 2023;28(9):2200535. DOI: https://doi.org/10.2807/1560-7917.ES.2023.28.9.2200535
Cheng K, Li J, Kong Q, Wang C, Ye N, Xia G. Risk factors for surgical site infection in a teaching hospital: a prospective study of 1,138 patients. Patient preference and adherence. 2015:1171-7. DOI: https://doi.org/10.2147/PPA.S86153
Aghdassi SJS, Schröder C, Gastmeier P. Gender-related risk factors for surgical site infections. Results from 10 years of surveillance in Germany. Antimicrobial Resistance & Infection Control. 2019;8:1-8. DOI: https://doi.org/10.1186/s13756-019-0547-x
Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R, et al. Diabetes and risk of surgical site infection: a systematic review and meta-analysis. infection control & hospital epidemiology. 2016;37(1):88-99. DOI: https://doi.org/10.1017/ice.2015.249
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA surgery. 2017;152(8):784-91. DOI: https://doi.org/10.1001/jamasurg.2017.0904
Dall’Era MA, Walsh TJ, Krieger JN. Infectious complications of urologic surgery. Complications of Urologic Surgery and Practice: Diagnosis, Prevention and Management New York: Informa. 2007:1-16. DOI: https://doi.org/10.3109/9781420013955-1
Walsh T, Dall’Era M, Krieger J. Preventing and Managing Infectious Emergencies of Urologic Surgery. Emergencies in Urology. 2007:430-43. DOI: https://doi.org/10.1007/978-3-540-48605-3_30
Hicks N, Gupta S. Complications and risk factors in elective benign scrotal surgery. Scandinavian journal of urology. 2016;50(6):468-71. DOI: https://doi.org/10.1080/21681805.2016.1204622
Patoir A, Payet C, Peix J-L, Colin C, Pascal L, Kraimps J-L, et al. Determinants of operative time in thyroid surgery: A prospective multicenter study of 3454 thyroidectomies. PLoS One. 2017;12(7):e0181424. DOI: https://doi.org/10.1371/journal.pone.0181424
Cheng H, Chen BP-H, Soleas IM, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration increases risk of surgical site infections: a systematic review. Surgical infections. 2017;18(6):722-35. DOI: https://doi.org/10.1089/sur.2017.089
Misha G, Chelkeba L, Melaku T. Incidence, risk factors and outcomes of surgical site infections among patients admitted to Jimma Medical Center, South West Ethiopia: Prospective cohort study. Annals of Medicine and Surgery. 2021;65:102247. DOI: https://doi.org/10.1016/j.amsu.2021.102247
Lilani S, Jangale N, Chowdhary A, Daver G. Surgical site infection in clean and clean-contaminated cases. Indian journal of medical microbiology. 2005;23(4):249-52. DOI: https://doi.org/10.1016/S0255-0857(21)02530-5
Darouiche RO, Wall Jr MJ, Itani KM, Otterson MF, Webb AL, Carrick MM, et al. Chlorhexidine–alcohol versus povidone–iodine for surgical-site antisepsis. New England Journal of Medicine. 2010;362(1):18-26. DOI: https://doi.org/10.1056/NEJMoa0810988
Luwang AL, Saha PK, Rohilla M, Sikka P, Saha L, Gautam V. Chlorhexidine–alcohol versus povidone–iodine as preoperative skin antisepsis for prevention of surgical site infection in cesarean delivery—a pilot randomized control trial. Trials. 2021;22(1):1-7. DOI: https://doi.org/10.1186/s13063-021-05490-4