Maintaining Normal Serum Ferritin Levels During Pregnancy: A Randomized Controlled Trial of Daily versus Weekly Ferrous Sulfate
Main Article Content
Abstract
Background:
Serum ferritin is the most reliable indication of stored iron in pregnancy, offering a noninvasive way to detect iron deficiency anemia before it occurs. Therefore, this study aimed to determine serum ferritin levels among women receiving daily versus weekly iron supplementation, with a secondary focus on comparing the proportion developing iron deficiency anemia and compli-ance rates between the two groups.
Methods:
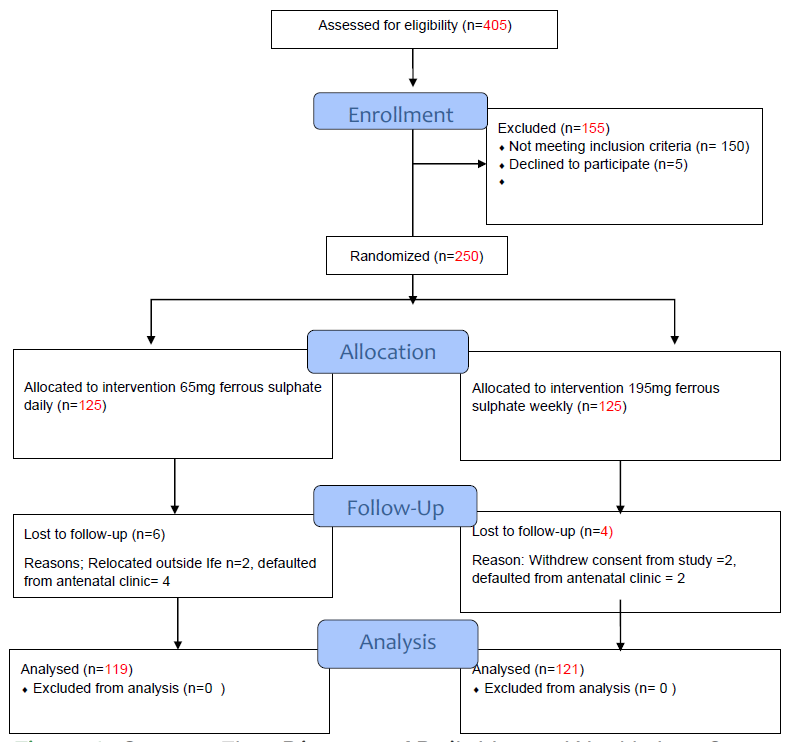
This non-blinded randomized control trial involved non-anaemic pregnant women attend-ing antenatal clinics at two Teaching Hospitals in Osun State. One hundred twenty-five subjects were recruited to receive 65mg in the control group, while another 125 subjects in the active group re-ceived three tablets (195mg) of ferrous sulfate (Fesulf) once weekly for 17 weeks from the 20th to 37th weeks of gestation. The primary outcome measure was comparing mean serum ferritin levels in both groups at 37 weeks.
Results:
Among the 240 subjects analyzed, the 37-week serum ferritin level was higher in the daily group (73.26±26.67μg/L) compared to the weekly group (63.04±30.71 μg/L), p value=0.006. Four (3.36%) and 10 (8.26%) of our subjects had Iron deficiency anaemia. Nine subjects (3.75%) reported dyspepsia as a side effect. Daily 65 mg of Felsulf proved more effective than weekly 195mg in main-taining normal blood ferritin levels during pregnancy.
Conclusions:
Daily iron supplementation with 65mg ferrous sulfate was more effective at main-taining adequate maternal iron concentration in this group of non-anaemic pregnant women. This dosage is recommended for routine iron supplementation in our environment.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) license. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
How to Cite
References
References
McLean E, Cogswell M, Egli I, Wojdyla D, De Benoist B. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993-2005. Public Health Nutr. 2009;12(4):444–54. DOI: https://doi.org/10.1017/S1368980008002401
Ajepe AA, Okunade KS, Sekumade AI, Daramola ES, Beke MO, Ijasan O, et al. Prevalence and foetomaternal effects of iron deficiency anaemia among pregnant women in Lagos, Nigeria. PLoS One. 2020;15(1):1–13. DOI: https://doi.org/10.1371/journal.pone.0227965
Nwizu EN, Iliyasu Z, Ibrahim SA, Galadanci HS. Socio-demographic and maternal factors in anaemia in pregnancy at booking in Kano, northern Nigeria. Afr J Reprod Health. 2011;15(4):33–41.
Ndukwu GU DPO. Prevalence and socio-demographic factors associated with anaemia in pregnancy in a primary health centre in Rivers state, Nigeria. Afr J Pri Health Care Fam Med. 2012;4(1):112–6. DOI: https://doi.org/10.4102/phcfm.v4i1.328
Ejiofor CC, Ozokono RU, Ugwu JI. Prevalaence of Anaemia among Preganant Women Attending 82 Division Nigerian Army Hospitals, Enugu. Gynecol Obstet Res. 2019;6(1):1–5. DOI: https://doi.org/10.17140/GOROJ-6-148
Kareem YO, Ameyaw EK, Bello OO, Abdus-Salam RA, Lawal OO, Obajimi G, et al. Ecological analysis of demographic-, nutritional- and housing-related factors associated with anaemia among women of reproductive age group in Nigeria. J Health Popul Nutr. 2022 Dec 9;41(1):56. DOI: https://doi.org/10.1186/s41043-022-00334-6
Pratt JJ, Khan KS. Non-anaemic iron deficiency - a disease looking for recognition of diagnosis: A systematic review. Eur J Haematol. 2016;96(6):618–28. DOI: https://doi.org/10.1111/ejh.12645
Adaji JA, Isah AY, Agida ET, Otu T, Abdullahi HI. Daily versus twice daily dose of ferrous sulphate supplementation in pregnant women: A randomized clinical trial. Niger J Clin Pract. 2019;22(8):1132–9. DOI: https://doi.org/10.4103/njcp.njcp_211_18
Garcia-Casal MN, Pasricha SR, Martinez RX, Lopez-Perez L, Peña-Rosas JP. Serum or plasma ferritin concentration as an index of iron deficiency and overload. Cochrane Database of Systematic Reviews. 2021;5(5). DOI: https://doi.org/10.1002/14651858.CD011817.pub2
Milman N, Taylor CL, Merkel J BPM. Iron status in pregnant women and women of reproductive age in Europe. Am J of Clin Nutr. 2017;106(6). DOI: https://doi.org/10.3945/ajcn.117.156000
Ogunbode O, Damole IO OOA. Iron supplement during pregnancy using three different iron regimens. Curr Ther Res Clin Exp. 1980;27:75–80.
Hwang JY, Lee JY, Kim KN, Kim H, Ha EH, Park H, et al. Maternal iron intake at mid-pregnancy is associated with reduced fetal growth: Results from Mothers and Children’s Environmental Health (MOCEH) study. Nutr J. 2013;12(1):1–7. DOI: https://doi.org/10.1186/1475-2891-12-38
Lao TT, Tam KF, Chan LY. Third trimester iron status and pregnancy outcome in non-anaemic women; Pregnancy unfavourably affected by maternal iron excess. Human Reproduction. 2000;15(8):1843–8. DOI: https://doi.org/10.1093/humrep/15.8.1843
Fasola FA, Anetor JI, Ilesanmi OS. An investigation of the prevalence of iron overload in Nigerian women. Afr J Med Med Sci. 2013;42(3):231–7.
Pena-Rosas JP, De-Regil LM, Dowswell T VFE. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2012;11(7). DOI: https://doi.org/10.1002/14651858.CD009997
World Health Organization. Guideline: Intermittent iron and folic acid supplementation in non‐anaemic pregnant women. Geneva: World Health O. Geneva; 2012.
Adanikin AI, Awoleke JO, Olofinbiyi BA, Adanikin PO, Ogundare OR. Routine Iron Supplementation and Anaemia by Third Trimester in a Nigerian Hospital. Ethiop J Health Sci. 2015;25(4):305–12. DOI: https://doi.org/10.4314/ejhs.v25i4.3
Kirkwood BR SJ. Essential medical statistics. 2nd ed. Kirkwood BR, Sterne JAC, editors. Oxford: Blackwell; 2003.
Van Den Broeck LWS. Iron status in pregnant women: which measurements are valid? . Br J Haematol. 1998;103:817–24. DOI: https://doi.org/10.1046/j.1365-2141.1998.01035.x
Pavord S, , B Myers, S Robinson, S Allard, J Strong CO. Real time conditioning monitoring for failure prediction. UK guidelines on the management of iron deficiency in pregnancy. 2011;1–34.
Daru J, Cooper NAM, Khan KS. Systematic review of randomized trials of the effect of iron supplementation on iron stores and oxygen carrying capacity in pregnancy. Acta Obstet Gynecol Scand. 2016;95(3):270–9. DOI: https://doi.org/10.1111/aogs.12812
Mei Z, Addo OY, Jefferds ME, Sharma AJ, Flores-Ayala RC BGM. Physiologically based serum ferritin thresholds for iron deficiency in children and non-pregnant women: a US National Health and Nutrition Examination Surveys (NHANES) serial cross-sectional study. Lancet Haematol. 2021;8(8). DOI: https://doi.org/10.1016/S2352-3026(21)00168-X
Van Den Broek NR, Letsky EA, White SA, Shenkin A. Iron status in pregnant women: Which measurements are valid? Br J Haematol. 1998;103(3):817–24. DOI: https://doi.org/10.1046/j.1365-2141.1998.01035.x
Georgieff MK, Krebs NF, Cusick SE. The Benefits and Risks of Iron Supplementation in Pregnancy and Childhood. Annu Rev Nutr. 2019;39:121–46. DOI: https://doi.org/10.1146/annurev-nutr-082018-124213
Hanieh S, Ha TT, Simpson JA, Casey GJ, Khuong NC, Thoang DD, et al. The Effect of Intermittent Antenatal Iron Supplementation on Maternal and Infant Outcomes in Rural Viet Nam: A Cluster Randomised Trial. PLoS Med. 2013;10(6). DOI: https://doi.org/10.1371/journal.pmed.1001470
Peña-Rosas JP, De-Regil LM, Gomez Malave H, Flores-Urrutia MC, Dowswell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews. 2015 Oct 19;2015(10). DOI: https://doi.org/10.1002/14651858.CD009997.pub2
Hemminki E, Rimpela U. Iron supplementation, maternal packed cell volume, and fetal growth. Arch Dis Child. 1991;66:422–5. DOI: https://doi.org/10.1136/adc.66.4_Spec_No.422
Percy L, Mansour D. Iron deficiency and iron‐deficiency anaemia in women’s health. The Obstetrician & Gynaecologist. 2017;19(2):155–61. DOI: https://doi.org/10.1111/tog.12368
Kassebaum NJ, Jasrasaria R, Johns N, Wulf S, Chou D, Lozano R, et al. A systematic analysis of global anaemia burden between 1990 and 2010. The Lancet. 2013;381:S72. DOI: https://doi.org/10.1016/S0140-6736(13)61326-4
Singh U, Singh S, Gupta HP, Natu SM, Deo S BS. Once a week (200mg) elemental iron: an effective option for prophylaxis in non-anaemic pregnant women. J Ind Med Assoc. 2011;109(9):654–6.
Meza-camacho C, Casanueva E, Viteri FE. Weekly Iron as a Safe Alternative to Daily Supplementation for Nonanemic Pregnant Women. Arch Med Res. 2006;37:674–82. DOI: https://doi.org/10.1016/j.arcmed.2005.11.011
Haider LM, Schwingshackl L, Hoffmann G, Ekmekcioglu C. The effect of vegetarian diets on iron status in adults: A systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2018;58(8):1359–74. DOI: https://doi.org/10.1080/10408398.2016.1259210
Pavord S, Myers B, Robinson S, Allard S, Strong J, Oppenheimer C. UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol. 2012;156(5):588–600. DOI: https://doi.org/10.1111/j.1365-2141.2011.09012.x
Milman N, Bergholt T, Eriksen L, Byg KE, Graudal N, Pedersen P, et al. Iron prophylaxis during pregnancy - How much iron is needed? A randomized dose-response study of 20-80 mg ferrous iron daily in pregnant women. Acta Obstet Gynecol Scand. 2005;84(3):238–47. DOI: https://doi.org/10.1111/j.0001-6349.2005.00610.x